Crohn's disease: causes and symptoms
What is Crohn’s Disease?
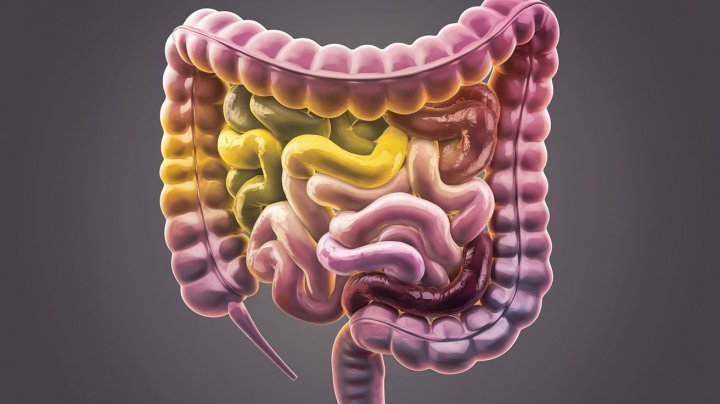
Crohn’s disease is a chronic,
inflammatory bowel disease (IBD) that can affect any part of the
digestive tract, leading to symptoms that range from mild to severe. As a
type of IBD, Crohn’s shares similarities with ulcerative colitis, yet
remains distinct in its manifestation and impact. Though it may develop
in anyone, a family history of the disease can increase your risk of
developing Crohn’s. Currently, there’s no cure for Crohn’s disease, but
early diagnosis and effective treatment can help manage symptoms and
improve quality of life. Let’s take a closer look at the causes,
symptoms, and treatment options available for Crohn’s disease.
Causes of Crohn’s Disease
The exact cause of Crohn’s disease remains unclear, but research suggests a combination of factors may contribute to its onset. These include genetic predisposition, environmental triggers, immune system responses, and certain lifestyle factors.
Genetic Factors
People with a family history of Crohn’s disease have a higher risk of developing the condition. Researchers have identified specific genes that may make some individuals more susceptible to inflammation in the digestive tract, which can lead to Crohn’s disease.
Environmental Triggers
Environmental factors, such as diet, smoking, and exposure to pollutants, may trigger Crohn’s disease in genetically predisposed individuals. Smoking, in particular, is associated with a higher risk of Crohn’s and may worsen symptoms.
Immune System Response
Crohn’s disease may result from an abnormal immune response that mistakenly attacks cells in the digestive tract, causing inflammation. This inflammation leads to the characteristic swelling and ulceration in the small intestine and large intestine, as well as around the anus.
Common Symptoms of Crohn’s Disease
Crohn’s disease symptoms can range from mild to severe, varying based on the location and extent of inflammation. The most common symptoms include abdominal pain, diarrhea, and weight loss. Many people with Crohn’s disease experience periods of remission followed by flare-ups, where symptoms become more severe.
-
Abdominal Pain and Cramping: Persistent abdominal pain is a hallmark of Crohn’s disease, often located in the lower right quadrant of the abdomen. This pain may intensify as inflammation worsens, making it difficult to carry out daily activities.
-
Diarrhea: Chronic diarrhea is another common symptom, often caused by inflammation in the digestive tract. Severe inflammation can lead to frequent, watery stools, which may be accompanied by urgency.
-
Fatigue: People with Crohn’s often feel fatigued due to the body’s ongoing inflammatory response and potential nutrient deficiencies caused by malabsorption.
-
Weight Loss and Reduced Appetite: Crohn’s can make it difficult for the body to absorb nutrients, leading to unintentional weight loss. Loss of appetite due to nausea or pain further compounds this issue.
-
Perianal Symptoms: Inflammation and swelling may occur around the anus, leading to discomfort, abscesses, or fistulas in more severe cases.
-
Additional Symptoms: Crohn’s disease may cause extra-intestinal symptoms, such as joint pain, skin rashes, and eye inflammation, which highlight the disease’s systemic nature.
Complications of Crohn’s Disease
Left untreated, Crohn’s disease can lead to serious complications. These may include:
-
Bowel Obstruction: Chronic inflammation can cause the walls of the digestive tract to thicken, leading to an obstruction that may require surgery to remove affected sections of the intestine.
-
Ulcers: Chronic inflammation in the digestive tract can cause open sores (ulcers) to form, which may occur anywhere from the mouth to the anus.
-
Fistulas and Abscesses: Severe inflammation can create abnormal connections, or fistulas, between the intestine and other organs or skin around the anus, leading to infections.
-
Malnutrition: Crohn’s disease may hinder nutrient absorption, increasing the risk of deficiencies in iron, calcium, and vitamin D.
Diagnosis and Tests for Crohn’s Disease
Diagnosing Crohn’s disease involves a combination of lab tests, imaging studies, and endoscopic procedures. Since no single test can confirm Crohn’s disease, a healthcare provider may recommend a range of tests to identify signs of inflammation, rule out other conditions, and confirm the diagnosis.
-
Blood Tests: Blood tests can check for markers of inflammation, anemia, or infection. Elevated levels of certain markers, like C-reactive protein (CRP), may indicate inflammation.
-
Stool Tests: Stool samples help detect signs of infection or inflammation in the digestive tract, which are common in IBD.
-
Endoscopy and Colonoscopy: An endoscopy examines the upper part of the digestive tract, while a colonoscopy visualizes the large intestine and sometimes the end of the small intestine. These procedures involve using a camera to detect signs of inflammation, ulcers, or other abnormalities.
-
Imaging Tests: Imaging techniques, such as CT scans or MRIs, may be used to obtain detailed pictures of the digestive tract, allowing for a more comprehensive assessment of inflammation and potential complications.
-
Capsule Endoscopy: Capsule endoscopy is a specialized test where a small capsule containing a camera is swallowed, capturing images of the small intestine as it travels through the digestive tract.
Treatment Options for Crohn’s Disease
Although there is currently no cure for Crohn’s disease, a variety of treatment options are available to help manage symptoms and reduce inflammation. Treatment plans are often personalized based on the severity of symptoms, the location of inflammation, and the individual’s response to medications.
Medications
Several medications can help control symptoms of Crohn’s disease, including anti-inflammatory drugs, immune system suppressors, and antibiotics.
-
Anti-Inflammatory Drugs: Corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to reduce inflammation. Corticosteroids are typically used for short-term flare-ups due to potential side effects.
-
Immune System Suppressors: These medications, such as azathioprine or biologics like infliximab, work by reducing the immune system’s response that contributes to inflammation. They are often used in individuals whose symptoms are severe or who don’t respond to other treatments.
-
Antibiotics: Antibiotics may be prescribed to treat abscesses, fistulas, or perianal infections associated with Crohn’s disease.
Lifestyle Modifications and Diet
A balanced diet and lifestyle changes can be highly effective in managing symptoms. Some individuals may benefit from keeping a food diary to identify potential dietary triggers.
-
Special Diet: Certain foods may trigger symptoms, so a low-residue or special diet can help reduce discomfort. Limiting fiber intake, avoiding fatty or fried foods, and reducing lactose consumption are common dietary recommendations.
-
Stress Management: Stress may worsen symptoms, so techniques such as mindfulness, yoga, or meditation can support symptom management.
Surgery
When medications and lifestyle modifications are not enough, surgery may be recommended. Surgery can involve removing damaged sections of the digestive tract, treating abscesses, or repairing fistulas. While surgery can relieve symptoms, it’s generally not considered a cure, as Crohn’s disease may recur in other parts of the digestive tract.
Managing Life with Crohn’s Disease
Living with Crohn’s disease requires consistent management and monitoring to maintain quality of life. The disease’s unpredictable nature means that individuals often need to adapt their routines, manage stress, and maintain a strong support network.
-
Monitoring Symptoms: Regular check-ups and communication with a healthcare provider are essential to monitor the disease’s progression and adjust treatment plans as needed.
-
Staying Informed: Reliable resources, such as the Crohn’s & Colitis Foundation, provide valuable information and support for those living with Crohn’s disease. They offer insights into research, clinical trials, and emerging treatment options.
-
Support Networks: Support from family, friends, or patient groups can make a significant difference in managing the psychological effects of Crohn’s disease.
Conclusion
Crohn’s disease is a chronic inflammatory bowel disease that causes inflammation in any part of the digestive tract. While the exact cause of Crohn’s disease remains unknown, factors such as genetics, immune response, and environmental influences are recognized as contributing factors. Symptoms like abdominal pain, diarrhea, and fatigue can vary in intensity, impacting daily life and increasing the risk of complications if left untreated.
Although there’s currently no cure, a combination of medications, lifestyle changes, and supportive therapies can help manage symptoms and reduce inflammation. Keeping a food diary, managing stress, and maintaining regular check-ups with a healthcare provider are key steps to living well with Crohn’s disease.
For those with Crohn’s, tools like the Chatdok app can offer valuable support. Chatdok provides personalized health insights and symptom tracking that can help individuals monitor changes in their condition and access health tips tailored to their needs. With Chatdok, people living with Crohn’s have the advantage of a digital companion to help manage their health daily.